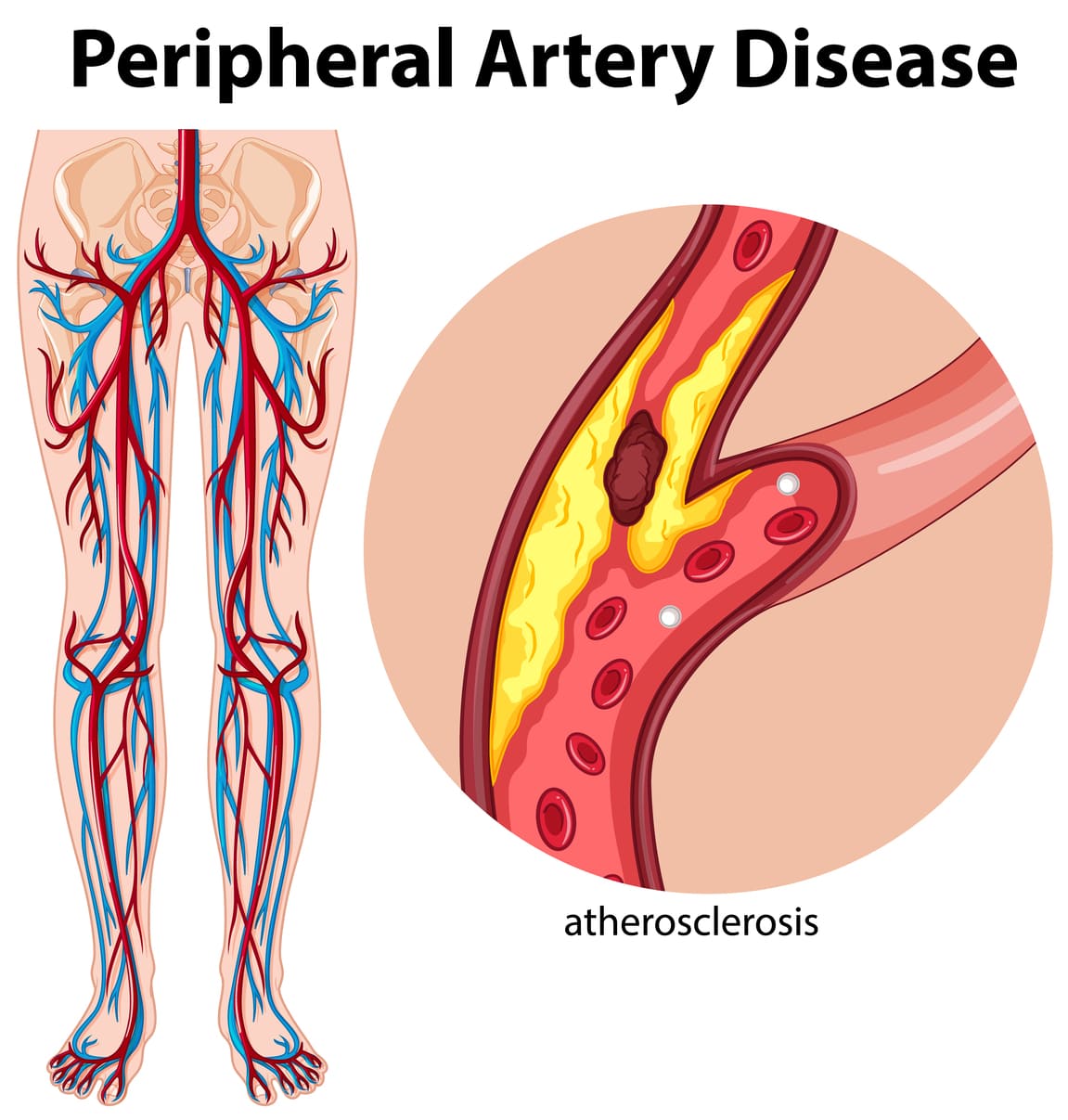
Peripheral artery disease (PAD) is when narrowed arteries reduce blood flow to the arms or legs. This can cause pain, numbness, weakness, and other discomforts. While PAD can affect anyone, research shows it has a more significant impact on specific ethnic groups, particularly Black Americans. This notable difference in how PAD affects people from different backgrounds shows a grave health inequality that needs urgent reforms.
Understanding the Disparity
The reasons behind this disparity are complex. These disparities arise from a complex biological, social, and environmental interplay. Biological causes, such as genetics, may contribute, but social and environmental influences play a much more significant role. These are often called social determinants of health, including income, education, access to healthcare, and living conditions.
For example, Black Americans are more likely to live in areas with fewer resources, including healthy food options, safe housing, and quality healthcare services. Living in such environments can lead to chronic stress, which hurts heart and blood vessel health. Over time, this increased stress can raise the risk of PAD.
The Impact of PAD
PAD can cause several serious health problems. Many people experience pain, cramping, or weakness in its early stages, especially during physical activity. Over time, it can lead to more severe issues, like poor wound healing, making even minor cuts or sores challenging to recover from. In the worst cases, untreated PAD may result in the need for limb amputation.PAD is closely connected to other severe conditions like heart disease and stroke. This implies that a patient with PAD is at a higher risk of developing a heart attack or stroke, and hence, critical early detection and management of the disease are essential.
The Role of Social Determinants of Health
Social factors play a significant role in PAD’s development and progression. Lower income levels and limited educational opportunities often result in less access to healthcare and a higher risk of PAD. When people do not have access to quality medical care, they may experience delays in diagnosing and treating the disease, which allows it to worsen over time. Environmental factors also play a part. For example, exposure to air pollution or a noisy environment can negatively impact blood vessels and circulation, increasing the risk of developing PAD. These issues often overlap, producing a cycle hard to break without broader systemic changes.
Managing PAD and Reducing Disparities
Managing PAD requires both prevention and treatment. Lifestyle changes like a healthy diet, regular exercise, quitting smoking, and stress management can improve blood flow and lower the risk of complications. Medications may also help with circulation, cholesterol, and clot prevention. At the same time, severe forms may necessitate either angioplasty or bypass surgery.
Eliminating inequalities is founded on understanding root causes: having access to adequate and affordable health care, providing early screenings, and raising awareness among less privileged populations about prevention and symptom recognition of PAD.
A Path Forward
Community-wide efforts will be needed to address the ethnic disparities in PAD. It includes steps such as handling reasons for why some people are way more susceptible to the disease than others, from the social and economic aspects. Making it into – more excellent healthcare in underserved areas – would make a difference. It’s also essential to address systemic problems, including racial bias in healthcare and policies that enforce equal treatment for all patients.